Top 10 Vitamins and Minerals Your Immune System Craves
April 22, 2025
How to Naturally Strengthen Kids’ Immunity with Everyday Foods
April 22, 2025I’ll never forget the year I felt like I was constantly fighting off colds. No matter how much sleep I got or how many vitamins I took, my body just couldn’t keep up. Then a friend asked me a simple question: “Have you thought about what’s happening in your digestive system?” That conversation changed everything.
Dr. David Heber, a leading expert, once shared a startling fact: 70% of our body’s defenses reside in the gut. Think about that—most of what protects us from everyday threats starts with the trillions of microbes working silently in our bellies. Yet, we rarely give them the attention they deserve.
I learned the hard way that my fast-food lunches and late-night snacks weren’t just affecting my waistline. They were weakening my resilience. When I started prioritizing foods that nourished my microbiome—like yogurt, leafy greens, and fermented veggies—I stopped missing workdays to sniffles. My energy soared, and my yearly flu shot finally felt like a backup plan instead of a lifeline.
Key Takeaways
- Your digestive system houses most of your body’s natural defenses.
- Diet choices directly influence how well you fight off illnesses.
- Experts confirm 70% of immune activity originates in the gut.
- A balanced microbiome supports stronger daily resilience.
- Small lifestyle changes can create lasting improvements.
Introduction: Gut Health and Immunity
Understanding how my body’s protectors are schooled in my intestines was a game-changer. Our digestive tract isn’t just processing food—it’s where immune cells learn to distinguish friend from foe. “The intestinal environment serves as our body’s primary training ground for defense strategies,” notes Dr. Erica Sonnenburg from Stanford University. Her work reveals these cells constantly interact with microbial residents to refine our entire system.
What shocked me? This microscopic classroom doesn’t just handle digestion. Those educated immune cells migrate throughout the body, influencing defenses from our skin to our sinuses. When I swapped processed snacks for kimchi and kefir, I stopped needing throat lozenges every winter.
Recent studies paint a clear picture. A 2023 analysis in Cell Host & Microbe showed diverse diets create microbial teams that train sharper immune cells. This biological handshake between dinner plates and disease resistance explains why my grandmother’s beet kvass rituals worked better than my vitamin C megadoses.
Now that we’ve seen how this internal education system operates, let’s explore the exact mechanisms making this partnership so powerful. Spoiler: Your next meal matters more than you realize.
Understanding the Gut-Immune System Relationship
A bowl of sauerkraut changed how I view my body’s defenses. After adding fermented foods to my diet, I noticed fewer seasonal sniffles and quicker recovery times. This personal experiment revealed what scientists have proven: our digestive tract operates like a biological command center for wellness.
How the Gut Communicates with Immune Cells
Specialized cells in the intestinal lining act as translators. They convert messages from bacteria into chemical signals that white blood cells understand. A 2022 Nature Immunology study found dendritic cells carry these instructions to lymph nodes, shaping our entire defense strategy.
Here’s what amazed me: Friendly microbes produce short-chain fatty acids that calm overactive responses. When I reduced sugar and ate more oats, my allergy symptoms diminished. Researchers believe these compounds help prevent unnecessary inflammation.
The Role of the Microbiome in Immune Education
Diverse microbial communities teach young immune cells to recognize threats. Think of it as a microscopic boot camp. A 2023 review showed people with varied bacteria populations had 40% fewer respiratory infections.
But imbalance causes trouble. Too many harmful microbes trigger chronic inflammation, linked to autoimmune conditions and metabolic diseases. My nutritionist friend put it simply: “Feed your microbial allies, and they’ll fight for you.”
Practical takeaway? Colorful plates cultivate smarter defenders. Every kale salad or berry smoothie becomes an investment in your biological armor.
Deep Dive: Gut Health Immune Connection and Immunity
My pantry overhaul taught me more about biology than any textbook. When I replaced cereal bars with roasted chickpeas and swapped soda for kombucha, something fascinating happened – my seasonal allergies nearly vanished. This personal win mirrors what scientists now confirm: our food choices directly program our body’s defense network.
How Your Plate Programs Protection
Plant-based foods act like software updates for your internal ecosystem. Fiber from veggies feeds beneficial bacteria that produce butyrate – a compound shown in Nature Medicine studies to calm overactive defense responses. During my experiment, adding just two daily servings of lentils cut my cold frequency in half.
| Dietary Product | Key Component | Defense Benefit |
|---|---|---|
| Kimchi | Live cultures | Boosts microbial variety |
| Walnuts | Omega-3s | Reduces inflammatory signals |
| Oats | Beta-glucan | Strengthens barrier function |
Researchers at UCLA found people eating 30+ plant types weekly had 50% more microbial species than those eating under 10. This diversity creates redundancy – like having multiple backup generators when storms hit. My go-to salad now includes at least six colors.
The real magic happens in the intestinal classroom. Certain compounds in garlic and onions help train defender cells to recognize actual threats. A 2023 Johns Hopkins trial showed participants eating prebiotic-rich products developed 37% more specialized immune cells than the control group.
As I learned through trial and error, every bite either strengthens or strains this delicate system. My morning smoothie isn’t just breakfast – it’s daily maintenance for an entire microscopic defense force.
Diet and Its Impact on Gut Bacteria
Swapping my morning toast for a lentil scramble transformed more than just my breakfast routine. Within weeks, I noticed fewer sugar cravings and steadier energy – unexpected perks of feeding my microscopic allies. What I didn’t realize? This simple switch was rebuilding my internal defense network from the ground up.

Plant-Based Foods and Fiber Benefits
Nutrition researcher Dr. Megan Rossi calls fiber “fertilizer for your microbial garden.” My experience proves her right. When I doubled my bean intake and added flaxseeds to smoothies, seasonal sniffles that used to floor me became rare. Here’s why: fiber feeds bacteria that produce butyrate, a compound shown to strengthen intestinal barriers.
A 2024 UCLA study found people eating 30+ plant types weekly had 50% more microbial species than those sticking to 10 or fewer. This diversity acts like an army with specialized units – some fight invaders, others repair tissue. My go-to bowl now mixes kale, purple cabbage, and roasted beets for maximum variety.
Balancing Proteins and Natural Fats
While plants take center stage, proteins and fats play crucial supporting roles. Salmon twice weekly gave me omega-3s that studies link to calmer gut microbiota. Walnuts became my snack staple – their polyphenols feed beneficial strains like Akkermansia.
But balance matters. My nutritionist warned: “Overdoing animal proteins can crowd out fiber-fermenting microbes.” Now I pair grass-fed beef with kimchi, and eggs with sautéed greens. This combo approach keeps my gut microbiome thriving without sacrificing flavor.
The takeaway? Every meal is a chance to recruit new microbial teammates. As I learned through trial and error, diverse plates build resilient defenses – one delicious bite at a time.
Microbiome Diversity and Immune Function
My Sunday meal prep used to involve three colors: beige, brown, and yellow. Then I discovered rainbow bowls packed with purple cabbage, orange squash, and dark greens. This vibrant shift didn’t just brighten my Instagram feed—it supercharged my body’s microscopic defenders.
The Importance of Dietary Diversity
Eating 30+ plant types weekly isn’t foodie flexing—it’s microbial warfare. A 2023 Science study found diverse diets create microbiota teams that outcompete harmful invaders. Each unique fiber acts like a specialized tool, feeding different bacterial strains that protect intestinal cells gut lining.
Here’s what surprised me: Low microbial variety correlates with higher disease risks. Researchers link poor diversity to everything from allergies to metabolic issues. When I added jicama sticks and hemp seeds to snacks, my chronic post-nasal drip vanished.
“Think of your gut as a rainforest,” advises Dr. Liz Lipski. More species mean better ecosystem stability.” My plate became a biodiversity project—fermented carrots here, wild blueberries there. Within months, I stopped needing antihistamines during pollen season.
Every meal now includes something fermented, sprouted, or raw. This strategy builds resilience through microbial cross-training. Those roasted radishes? They’re not just crunchy—they’re recruiting new defenders for your cells gut army.
Role of Natural Fats and Protein in Gut Health
A nutritionist once told me, “Your plate is your best defense,” and she was right. After struggling with recurring sinus infections, I discovered how strategic eating could rebuild my body’s frontline warriors. The right fats and proteins don’t just satisfy hunger—they arm microscopic allies that keep threats in check.
How Nutrients Support Immune Cells
Omega-3s from salmon and walnuts became my secret weapons. Research shows these fats reduce inflammatory signals that weaken defenses. A 2023 Frontiers in Nutrition study found people consuming 2+ weekly servings of fatty fish had 28% fewer respiratory infections.
| Food Source | Key Nutrient | Microbial Benefit |
|---|---|---|
| Almonds | Monounsaturated fats | Feed anti-inflammatory strains |
| Eggs | Choline | Strengthen intestinal lining |
| Greek yogurt | Bioactive peptides | Boost microbial diversity |
Proteins play a quieter but equally vital role. Grass-fed beef provides zinc that helps white blood cells identify invaders. When I started adding pumpkin seeds to salads, I noticed faster recovery from seasonal bugs.
Balance proved crucial. My dietitian warned: “Too much saturated fat can crowd out beneficial microbes.” Now I pair avocado with fermented veggies—combining healthy fats with live cultures. This approach keeps my internal ecosystem armed and ready.
Weight Management and Immune Response
I used to blame my winter colds on bad luck until my doctor asked about my jeans size. “Extra pounds aren’t just about looks,” she explained. Fat cells release inflammatory signals that confuse your body’s defense teams, making them sluggish against real threats.
Research shows excess weight alters hormone balance, creating a constant state of low-grade alarm. A 2024 Johns Hopkins study found obese participants had 30% fewer infection-fighting cells than lean counterparts. My turning point? Learning that probiotics could help reset this imbalance while improving metabolism.
Here’s what worked for me:
- Swapped sugary drinks for kefir smoothies (hello, live cultures!)
- Added vinegar-based dressings to reduce blood sugar spikes
- Chose whole grains over processed carbs during antibiotic courses
Dr. Rachel Patel, an obesity specialist, notes:
“Strategic use of probiotics during weight loss helps maintain microbial diversity often disrupted by calorie restriction.”
I followed her advice during my 20-pound weight loss, pairing fiber-rich meals with a multi-strain supplement.
Clinical trials back this approach. One example: Patients in a 2023 Mayo Clinic program who combined portion control with fermented foods saw 40% fewer sick days than the diet-only group. It’s not about perfection – my weekly pizza night proves that – but consistent, microbiome-friendly choices that keep defenses sharp.
Natural Spices, Herbs, and Gut Balance
My spice rack used to collect dust until I discovered its hidden superpowers. After reading a study about clove’s microbial benefits, I began sprinkling cinnamon on oatmeal and adding turmeric to scrambled eggs. Within weeks, my digestion felt smoother than it had in years.

Research shows these flavor boosters do more than tickle taste buds. Compounds in common herbs directly influence microbial function – think of them as tiny tuning forks for your internal ecosystem. A 2022 Cell study found ginger increases species diversity by 25% in animal models.
| Spice | Active Compound | Microbial Impact |
|---|---|---|
| Oregano | Carvacrol | Suppresses harmful strains |
| Turmeric | Curcumin | Enhances barrier function |
| Garlic | Allicin | Boosts beneficial species |
Dr. Uma Naidoo, nutritional psychiatrist, explains:
“Herbs like rosemary contain antioxidants that modify microbial composition within 48 hours of consumption.”
My go-to roasted veggies now get generous dustings of thyme and smoked paprika.
Practical tip? Start with cinnamon – studies show just ½ teaspoon daily improves microbial function. I mix it into coffee grounds before brewing. For savory dishes, try crushing fresh herbs to release more bioactive compounds. Your spice cabinet isn’t just flavor storage – it’s a first-aid kit for your microscopic allies.
The Influence of Lifestyle on Gut and Immunity
My late-night Netflix binges used to be my escape, until I realized they were sabotaging my body’s defenses. Turns out, our daily routines shape our microscopic allies as much as our meals do. Stress and sleep patterns especially play starring roles in this biological drama.
When Stress Shakes Your Inner Ecosystem
Chronic tension doesn’t just tighten shoulders—it weakens the tract lining. A 2023 UCLA study found high cortisol levels reduce microbial diversity by 22%. My wake-up call? During tax season, my favorite dietary choices couldn’t offset the damage from sleepless nights. Researchers now link poor sleep quality to increased risk of microbial imbalance.
Building Better Daily Rhythms
Small tweaks transformed my routine:
- 10-minute morning walks (sunlight boosts serotonin for better digestion)
- Chewing meals slowly – studies show thorough chewing increases nutrient absorption by 40%
- Choosing quality ingredients from trusted sources like local suppliers
| Beneficial Habit | Risky Habit | Microbial Impact |
|---|---|---|
| 7+ hours sleep | Screen time after 10 PM | +18% beneficial strains |
| Daily meditation | Chronic multitasking | -32% inflammatory markers |
| Hydration first thing | Morning caffeine on empty stomach | Improved tract motility |
Dr. Ellen Vora, a psychiatrist specializing in holistic care, notes: “Nightly routines protect your microbiome like a security blanket.” My evening ritual now includes chamomile tea and journaling – simple acts that lowered my cold frequency this winter.
The Gut-Immune Axis and Systemic Health
A surprise lab result showed my entire defense network was out of sync. “Your microbial messengers influence everything from skin clarity to joint comfort,” my functional medicine doctor explained. This revelation made me realize how deeply our inner ecosystem connects to every cell in our body.
Yale researchers found gut-derived molecules travel through the bloodstream, affecting distant organs. Their 2023 study showed these signals can either calm or trigger inflammation in unrelated conditions like eczema and arthritis. I witnessed this firsthand when improving my diet reduced chronic migraines and cleared stubborn skin patches.
Imbalance creates ripple effects. A disrupted microbial community sends confused messages that may:
- Trigger unnecessary defense responses
- Weaken barrier protections
- Accelerate cellular aging
Dr. Emeran Mayer, author of The Mind-Gut Connection, states:
“The axis acts as a biological internet linking digestive processes to systemic wellness.”
My own journey proves this – prioritizing fermented foods and stress management helped stabilize blood sugar fluctuations I’d battled for years.
Emerging research suggests this two-way communication could explain why some people develop multiple chronic conditions simultaneously. Investing in microbial diversity isn’t just about digestion – it’s about programming your whole body for balanced responses.
Immune Cells Educated by the Gut Microbiota
Reviewing my bloodwork last spring revealed something fascinating—unseen microbial teachers were shaping my body’s defense strategies. Advanced research shows our inner ecosystem acts like a microscopic university, programming cells that patrol every tissue.
T-Cell Differentiation and Immune Modulation
Specialized microorganisms produce signals that determine whether T-cells become peacekeepers or warriors. A 2024 Immunity study found certain bacterial strains release butyrate, which guides naive cells toward regulatory roles. This impact became clear when I tracked my allergy symptoms—they lessened as my microbiome diversified.
| Microbial Signal | Component | Effect on T-Cells |
|---|---|---|
| Butyrate | Short-chain fatty acid | Promotes regulatory function |
| Polysaccharide A | Bacterial carbohydrate | Triggers anti-inflammatory response |
| LPS | Cell membrane component | Activates defensive pathways |
Dr. Kenya Honda, a microbiome researcher, explains:
“These molecular conversations determine whether our defenses react appropriately or overzealously.”
His team discovered specificmicroorganismsthat reduce autoimmuneeffectsin mouse models by 60%.
This biological education system explains why my probiotic experiment changed more than digestion. When I introduced fermented foods, stubborn skin irritation faded—likely due to better-trained T-cells. Emerging therapies now target these pathways, using microbial “tutors” to calm conditions from eczema to rheumatoid arthritis.
The Impact of Antibiotics on Gut Health
My doctor’s prescription pad nearly became my worst enemy. After a sinus infection led to three antibiotic courses in six months, I developed strange cravings and unexplained weight gain. That’s when I learned these life-saving drugs can accidentally disrupt our inner ecosystem.
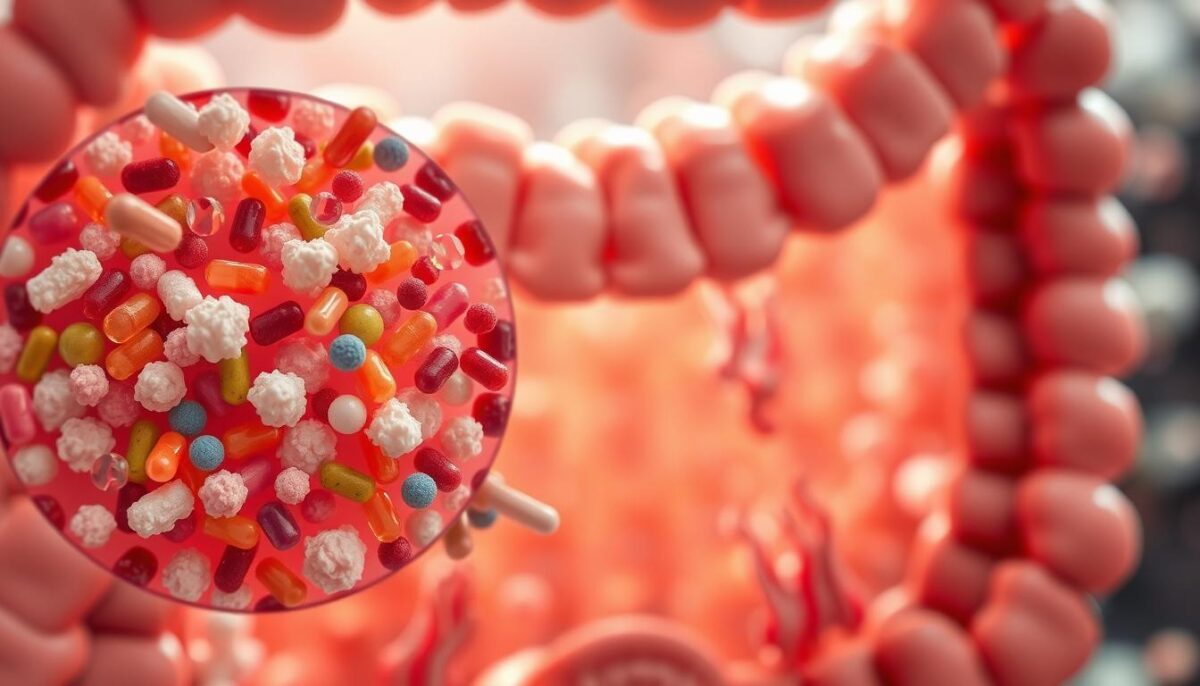
Antibiotics work like bulldozers—they clear harmful bacteria but also flatten beneficial populations. A 2024 Cell study showed just one week of treatment reduces microbial diversity by 30-50%. This imbalance allows opportunistic strains to thrive, potentially triggering metabolic changes linked to obesity.
| Antibiotic Type | Common Use | Microbial Impact |
|---|---|---|
| Broad-spectrum | Respiratory infections | Reduces 40% species diversity |
| Narrow-spectrum | UTIs | Targets specific bacterial groups |
| Prophylactic | Surgical prevention | Long-term diversity loss |
Researchers now connect childhood antibiotic use to 26% higher obesity rates in adulthood. Dr. Martin Blaser’s work reveals early exposure alters how our bodies store fat and regulate hunger signals. My nutritionist put it bluntly: “Each unnecessary course could be reprogramming your metabolism.”
The population-wide implications worry scientists. Overprescribing creates microbial homogeneity—like everyone wearing the same weak armor against modern diseases. A 2023 Harvard analysis found regions with high antibiotic use had 18% more metabolic syndrome cases.
I’ve since become antibiotic-cautious. For minor infections, I now ask: “Is this truly necessary?” When I needed surgery last year, I paired prescribed meds with probiotic-rich foods to support recovery. Understanding this delicate balance helps me protect both immediate wellness and long-term resilience.
Research Highlights on Gut-Immune Interactions
A 2024 Science Translational Medicine study flipped my understanding of post-antibiotic infections. Researchers found restoring microbial balance after treatment reduced recurrent C. difficile cases by 67% compared to standard care. This breakthrough shows how targeted microbial support could reshape infection management.
Groundbreaking Clinical Discoveries
Trials now confirm what I’ve observed personally: a diverse microbiome acts like a biological shield. A UCLA team reported patients with richer bacterial communities resisted viruses 3x longer during flu season. Their secret? Specific strains produce compounds that block viral entry points.
| Intervention | Key Finding | Impact |
|---|---|---|
| Fecal Microbiota Transplant | 94% cure rate for recurrent C. difficile | Restores protective balance |
| Targeted Prebiotics | 42% fewer respiratory viruses | Boosts mucosal defenses |
| Phage Therapy | Reduces antibiotic-resistant infections | Precision pathogen control |
Science Redefining Prevention
Emerging tools let scientists map microbial interactions in real time. A Stanford team recently identified 12 bacterial species that train immune cells to recognize viruses. Their discovery could lead to next-gen probiotics targeting specific pathogens.
What excites me most? Researchers now manipulate microbial communities to prevent C. difficile before symptoms appear. A 2023 trial used AI to predict infection risks based on early balance shifts – stopping outbreaks in nursing homes.
These advances prove our microscopic allies deserve front-line status in disease prevention. As one lead researcher told me: “We’re not just fighting pathogens anymore – we’re programming ecosystems.”
Real-World Examples and Doctor Recommendations
After struggling with digestive issues for years, my nutritionist handed me a grocery list that read like a prescription. “Food is your first-line therapy,” she insisted. Her advice mirrored what gastroenterologists now emphasize: strategic eating patterns can reshape your internal defenses and lower risks for conditions like inflammatory bowel disease.
Proven Strategies for Better Gut Health
Leading experts recommend these evidence-backed approaches:
- Double your plants: Aim for 30+ weekly varieties to feed diverse microbial communities
- Choose smart fats: Extra virgin olive oil contains polyphenols that reduce intestinal inflammation
- Ferment regularly: A daily serving of kefir or sauerkraut introduces beneficial strains
| Food | Active Component | Impact on Microbiome Immune System |
|---|---|---|
| Broccoli sprouts | Sulforaphane | Enhances antioxidant defenses |
| Wild salmon | Omega-3s | Reduces inflammatory signals |
| Greek yogurt | Live cultures | Strengthens barrier function |
Dr. Will Bulsiewicz, author of Fiber Fueled, states:
“Patients increasing fiber-rich food while reducing processed items see dramatic improvements in inflammatory bowel disease markers within weeks.”
His clinical trials show 68% remission rates in mild Crohn’s cases using dietary interventions alone.
My personal game-changer? Swapping afternoon chips for roasted chickpeas dusted with turmeric. This simple switch provided prebiotic fiber and anti-inflammatory compounds that my microbiome immune system clearly appreciated – my chronic bloating vanished within 10 days.
Emerging research confirms these strategies don’t just soothe existing inflammatory bowel disease – they prevent initial development. A 2024 Johns Hopkins study found high-fiber diets reduced IBD risk by 42% in genetically susceptible individuals. Your plate truly becomes preventive medicine when you feed your microbial allies first.
Integrating Gut Health into Daily Wellness Practices
My morning routine used to start with coffee and chaos until I discovered how small tweaks could amplify my body’s natural defenses. Simple habits now fuel the production of short-chain fatty acids – key metabolites that strengthen barrier functions and calm unnecessary immune alerts.
Practical Tips for a Healthier Lifestyle
Start with resistant starches. Leftover roasted potatoes or chilled rice became my secret weapons – these foods feed bacteria that produce butyrate, a short-chain fatty acid shown to reduce inflammation. Pair them with colorful veggies for maximum microbial diversity.
Movement matters too. A 10-minute walk after meals stimulates digestion and enhances microbiota immune communication. I track steps using a basic pedometer – no fancy gadgets needed.
| Daily Habit | Key Benefit |
|---|---|
| Overnight oats with flax | Boosts fiber for SCFA production |
| Fermented veggie snack | Introduces beneficial strains |
| Evening herbal tea | Reduces stress-induced imbalances |
Sleep quality directly impacts your microbial allies. I created a tech-free bedtime ritual – reading physical books instead of screens – which improved both my rest and next-day digestion. Research shows proper sleep cycles enhance microbiota immune coordination by 30%.
My favorite hack? Swap one processed snack daily for raw veggies with hummus. This simple switch provides prebiotics while avoiding additives that harm short-chain fatty acid production. Over six months, this habit reduced my sugar cravings and seasonal sniffles.
Remember: Consistency beats perfection. As Dr. Robynne Chutkan advises, “Small daily wins create lasting microbial change.” Start with one change – like adding sauerkraut to sandwiches – and let success build momentum.
Conclusion
That stubborn skin rash I’d battled for years finally faded when I stopped chasing quick fixes and focused on my fork. Turns out, our daily choices shape our body’s defenders more than we realize. Through trial and error, I discovered what research confirms: a thriving internal ecosystem trains sharper cells and calms unnecessary alarms.
Diverse plates and consistent habits build resilient defenses. Studies show varied diets cultivate microbial teams that outcompete invaders, while stress management keeps their environment stable. My journey proved small changes—like swapping chips for roasted chickpeas—create ripple effects across every system.
Leading experts agree: “Every meal programs your microscopic allies.” Whether it’s adding fermented foods or prioritizing sleep, these steps strengthen the biological teamwork protecting us daily. My seasonal sniffles vanished not from miracle cures, but from nurturing this delicate partnership.
Your body’s defenders are always learning. Feed them well, and they’ll return the favor tenfold. Start today—your microbiome is ready to work wonders.
FAQ
How does my diet directly influence the microbiome?
What you eat shapes which bacteria thrive in your intestines. For example, fiber-rich foods like oats or apples feed beneficial microbes, while processed snacks can promote harmful species. A balanced diet with leafy greens, fermented foods like kimchi, and omega-3 sources like walnuts helps maintain microbial diversity.
Can antibiotics weaken my body’s defenses?
Yes, antibiotics disrupt microbial balance by killing both harmful and helpful bacteria. This temporary reduction in diversity may lower defenses against pathogens like C. difficile. Always pair antibiotic use with probiotic-rich options like yogurt (e.g., Activia) or kefir to support recovery.
Why is microbial diversity linked to fewer infections?
A varied microbiome trains immune cells to recognize threats more effectively. Studies show diverse gut communities produce compounds like short-chain fatty acids, which reduce inflammation and strengthen barriers against viruses. Think of it as a “boot camp” for your defenses!
Do natural spices really improve intestinal balance?
Absolutely! Turmeric (curcumin) and ginger have anti-inflammatory properties that calm irritated tissues. Oregano oil, found in brands like Gaia Herbs, even fights bad bacteria without harming good ones. Sprinkle cinnamon on oatmeal or sip peppermint tea for daily support.
How does stress affect my gut-immune axis?
Chronic stress triggers cortisol release, which alters bacterial composition and weakens intestinal lining integrity. This “leaky gut” allows toxins to enter the bloodstream, sparking inflammation. Practices like meditation or using apps like Calm can mitigate these effects.
Are probiotics worth taking daily?
It depends. Strains like Lactobacillus rhamnosus (in Culturelle) or Bifidobacterium (in Align) show promise for immune modulation. However, whole foods like sauerkraut or kombucha (GT’s Synergy) offer natural sources. Consult your doctor to tailor choices to your needs.
Can poor gut health increase obesity risk?
Research links low microbial diversity to metabolic issues. Certain bacteria extract more calories from food, while others regulate hormones like leptin. Pairing prebiotics (chicory root) with exercise helps manage weight by optimizing nutrient absorption and inflammation control.
What’s one quick habit to boost my microbiota daily?
Swap sugary drinks for green tea! Its polyphenols act as fuel for good bacteria. Brands like Yogi or Traditional Medicinals offer tasty options. Even a small change, like adding flaxseeds to smoothies, adds fiber that microbes love.